The Delta variant factors are the dominant issues affecting travel today.

The Delta variant is more than 200 times more infectious than other COVID strains. Travelers must consider the Delta variant factors when deciding if and when they travel during the pandemic.
By July, the Delta variant accounted for 83 percent of analyzed COVID-19 cases in America. Due to the highly infectious Delta variant factors, travelers are questioning if we can continue to journey safely.
There is no easy answer to that question. Each of us must analyze our travel risk in order to decide if and when we can travel. Factors to consider include COVID facts ascertained from public health experts. Vulnerability to COVID, data on transportation modes, destinations, and COVID mitigation protocols must be examined.
Here is a list of critical factors to assist with travel decisions during the pandemic.
Delta variant data:
- The Delta variant is more than 200 percent more contagious than the original deadly COVID virus.
- While more investigation is needed, data from studies in Canada and Scotland show that the Delta variant causes more severe illness than previous strains of the virus and patients are more likely to be hospitalized if infected with Delta.
- Unlike in prior strains of COVID, both vaccinated and unvaccinated people infected with Delta are equally likely to infect others around them because they both have the same high levels of virus.
COVID-19 vaccination is the most effective means of preventing COVID infection.
COVID-19 vaccine information:
- Currently, the COVID vaccines used in the U.S. aren’t perfect in preventing infection. However, they are highly effective in preventing severe disease and death from COVID, including against the Delta variant.
- Based on CDC data, the COVID vaccines used in the U.S. are highly effective in substantially limiting the spread of COVID, including the Delta variant.
- Study after study shows that COVID vaccines are extremely safe and far more effective than first thought.
People with a serious risk from COVID-19 include:
- Those with systemic health conditions, cancer, chronic kidney, lung and heart conditions, diabetes, obesity, and other chronic diseases,
- Immuno-suppressed and immuno-compromised individuals,
- Senior citizens. (The risk increases with age.).
In addition to vaccination, wearing a face mask is an effective method of preventing COVID infection. It also prevents the transmission of the disease to others.
Protocol and methods to reduce the risk of contracting COVID or mitigate the effects of the virus:
- We know from studies that the COVID vaccines are the most effective way to prevent contracting the disease and lessening its effects if infected. A clear real-world indicator of that fact is that as of early August, 97 percent of those hospitalized for COVID in the U.S. were unvaccinated.
- According to the paper, “Effectiveness of Mask Wearing to Control Community Spread of SARS-CoV-2,” published in the Journal of the American Medical Association (JAMA) in February, wearing a face mask substantially reduces transmission of COVID-19. It does so by “blocking exhalation of virus-containing droplets into the air,” by as much as 50–70 percent, according to the type of mask, and forming a “barrier to large respiratory droplets.”
Whether vaccinated or not, avoiding travel to COVID hot spots is an important decision in preventing travelers from becoming infected with COVID.
There are COVID infection hot spots in the U.S. and across the globe:
- In the U.S., according to an analysis of the data at “WorldOMeter,” hot spots can be severe. The case surge in states like Florida, Louisiana, and Mississippi is so severe that they rank among the worst outbreaks of COVID-19 in the world.
- Outside of the U.S., current COVID-19 hot spots include France, Iceland, Spain, Greece, and others.
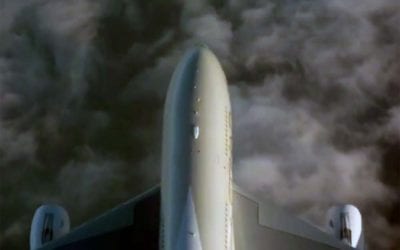
Car travel and short-distance air travel are among the safest modes of transportation to prevent contracting COVID-19 while traveling.
Transportation and COVID:
- Air travel for shorter distances, such as flying domestically, is generally safer than most other transportation modes. The air in plane cabins is filtered and changed many times per hour. “It takes the ventilation system of a plane about six minutes to reduce the number of viral particulates in the air by 99.9 percent.”
- Car travel is likely the safest mode of travel, as you’re generally only with members of your own household. Travel by personal car is safest, but rental cars are generally safe. Air a rental car out before driving. Wipe down inside surfaces with an alcohol wipe.
- Cruise travel is a major question at this point, for me. I enjoy cruising, but almost daily I read reports about the crew and passenger COVID infections on cruises. A recent Carnival cruise had 27 people test positive for COVID. It’s hard to pin down the safety of cruises with so many different cruise line protocols and requirements of port countries.
Here’s my take:
There are other COVID factors, of course. Hotels, local transportation at destinations, tours, and restaurant protocols, are all important. After traveling carefully since mid-July, I can’t recommend travel for anyone who’s not yet vaccinated, due to its high risk.
I’m holding off from cruising for now. Also, I avoid long flights typically needed for international travel. With the potential of sitting next to infected passengers for hours, plus other factors, I’m staying in the U.S. for now. Wear a face mask whenever inside public areas. Eat outside in restaurants. And, choose destinations carefully to avoid hot spots. If you’re vaccinated and careful about your decisions and conduct, a risk analysis may say it’s okay for you to travel, too.
After many years working in corporate America as a chemical engineer, executive and eventually CFO of a multinational manufacturer, Ned founded a tech consulting company and later restarted NSL Photography, his photography business. Before entering the corporate world, Ned worked as a Public Health Engineer for the Philadelphia Department of Public Health. As a well known corporate, travel and wildlife photographer, Ned travels the world writing about travel and photography, as well as running photography workshops, seminars and photowalks. Visit Ned’s Photography Blog and Galleries.